The Malaria Vaccine in Nigeria: The Long Journey Here, and the Rocky Road Ahead
Malaria is a disease that has plagued mankind since the beginning of time. Once a “death sentence”, this ubiquitous ague puzzled physicians for ages, so much that it was once attributed to bad air (as evidenced by its name), before it was discovered that it was caused by mosquitoes in the 19th century.
Two centuries later, malaria remains a killer disease, with an estimated 249 million malaria cases and 608 000 malaria deaths in 85 countries. Africa is home to 94% of these cases (233 million) and 95% of the deaths. Nigeria in particular, is the malaria capital of the world, shouldering 27% of the global malaria burden and 31% of malaria deaths worldwide. Most of these were pregnant women and children under the age of five. In fact, UNICEF estimates that nearly every minute, a child under 5 dies of malaria. This translates into the death of 1,000 children under age 5 every day.
Beyond the death toll, Africa loses billions of dollars every year in productivity and health expenses. The Malaria Consortium estimates that Africa loses $US 12 billion in Gross Domestic Product (GDP) every year. With malaria accounting for up to 40% of public health expenditure in some countries, it is no surprise that it has slowed economic growth in Africa by 1.3 percent per year. Economists call this a “growth penalty”; a chronic vicious cycle that ensures that poor countries only get poorer, and less able to control malaria.
The discovery of artemisinin-based combination therapies (ACTs) revolutionised the treatment of malaria. Gone were the days of chloroquine and quinine with their attendant cascade of side effects; the small yellow Coartem™ tablets took over the scene. Faster to act, highly effective, and with minimal side effects, they naturally became the drug of choice. ACTs have undergone an astounding metamorphosis. Once an exclusive preserve of large name-brands; they are now available in infinite forms and brands, each modified for better experience for the user. But despite malaria being so treatable, millions die every year. It is evident that malaria is a public health emergency in Africa; one that must be tackled on all fronts.
The Malaria Vaccines
Inspired by the remarkable success of vaccines against polio, measles, diphtheria, tetanus, and the eradication of small pox, scientists set out to create a vaccine for malaria in the 1960s. The Plasmodium parasite’s complex biology, life cycle and genome and its tendency to evade the human immune system made this a daunting task. With a multi-stage life cycle, and the ability to change its protein clothing to hide from the human immune system, developing a vaccine against it proved to be incredibly challenging.
In a historic development, scientists at GlaxoSmithKline (Gsk) created the first malaria vaccine (RTS,S/AS01) in 1987. Decades of clinical trials later, the WHO finally recommended the vaccine in 2021. Vaccinations began in three African countries; Ghana, Kenya, and Malawi. So far, a 13% drop in mortality among children eligible for the vaccine has been recorded, along with a marked reduction in severe malaria hospitalizations. The introduction of RTS,S set a precedent for malaria vaccines in endemic regions. However, producing the vaccine proved to be tedious and expensive; not only could GSK not meet the need for the vaccine, the countries that needed the vaccine most could not afford it, even with contributions from donors.
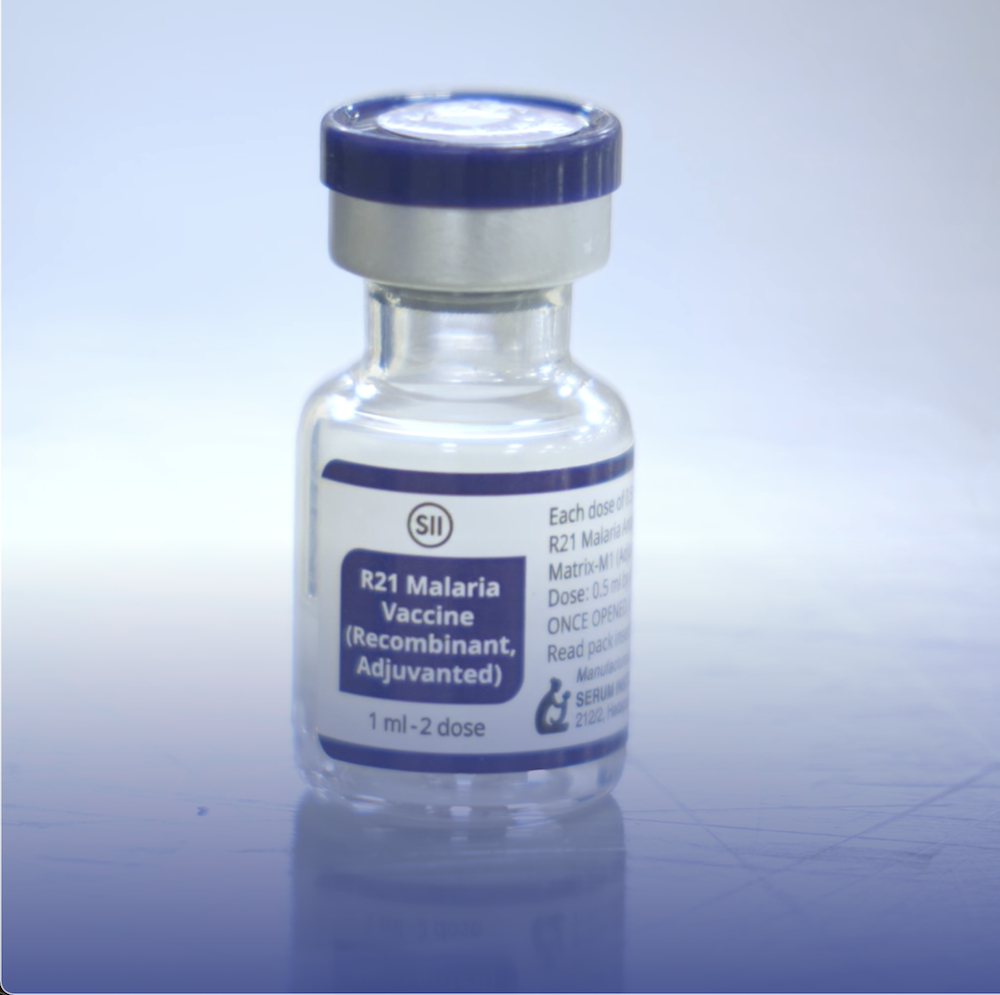
Thankfully, the R21 /Matrix-M vaccine was developed the Jenner Institute at Oxford University. At a third of the price of RTS,S, it had the same mechanism of action and about the same efficacy (75%). Production was also faster as the vaccine was easier to manufacture, with production being scaled up by the Serum Institute of India (SII) which has committed to producing up to 200 million doses annually. SII has also announced a technology transfer deal to produce the vaccine in Ghana. It is expected that a manufacturing facility will be completed in Accra soon. This would close the huge demand-supply gap.
Côte d’Ivoire and the Democratic Republic of Congo were among the first to roll out the vaccine. Having matched the cost and level of demand, the Global Alliance for Vaccines and Immunization (GAVI) considered the R21 vaccine best suited for Nigeria. However, a late application by Nigeria delayed the arrival of the vaccine in the country. Eventually, the first batch of 846,000 doses of the R21 malaria vaccine arrived Nigeria in October 2024. The vaccine was rolled out first to the states with the highest prevalence rates (Kebbi and Bayelsa). The National Primary Healthcare Development Agency (NPHCDA) promptly adjusted the National Programme on Immunization (NPI) schedule to include the vaccine, which is to be administered to infants between the age of 5 and 15 months.
Mechanism of Action
The R21 /Matrix-M targets the sporozoite stage of the Plasmodium falciparum life cycle by boosting the immune system’s response to circumsporozoite protein (CSP); the protein that enables sporozoites to invade liver cells. As this is the stage injected by mosquitos, it effectively nips it in the bud. The sporozoites that manage to break through are targeted by T cells, which are also activated by the vaccines.
The vaccine contains fragments of CSP linked to a protein from the hepatitis B virus that naturally self-assembles into virus-like particles – yet are completely harmless. By linking CSP to the highly antigenic protein from hepatitis B, a stronger immune response is induced. This clever structure is what makes the malaria vaccines the first effective vaccines to be developed against a parasite.
Trials have demonstrated that the vaccine is well tolerated and has a good safety profile, with injection site pain and fever being the most frequent adverse events. The protection conferred by the vaccine wanes over time, but the RTS,S vaccine is protective for up to seven years. This covers the period in life when children are most vulnerable. The duration of protection of R21 is not known yet, but it is expected to be similar.
Since humans and mosquitoes are the only hosts for Plasmodium falciparum, the less people are infected with the parasite, the better for everybody. With the right implementation, herd immunity from malaria may just be possible.
A Rocky Road for Nigeria
While the efficacy of the R21 vaccine is not in question, how it would play out in Nigeria remains to be seen. Nigeria’s health landscape is complicated by ignorance, vaccine hesitancy, an inverted healthcare pyramid, and logistics issues. Health expenditure is abysmally low. Perhaps without the combined efforts of GAVI, the Vaccine Alliance, UNICEF and WHO, the vaccine would have been out of reach.
For starters, the vaccine is given in four doses; the highest of any injectable vaccine in the National Programme on Immunization (NPI) schedule. The first three doses are given at five, six and seven months. A final booster dose is given at 15 months. Long immunization clinic wait times, pose a challenge for parents and caregivers who would now have to come every month for three months, in addition to the other vaccines that are scheduled at a different time. For those that live in remote locations, travelling long distances over unnavigable terrain and poor access roads discourages attendance. It so bad that a study shows that 9 in every 10 children who live in economically disadvantaged communities and states are not fully immunized. Ironically, these are the areas that need the vaccine most because of environmental conditions that encourage preponderance of mosquitoes. Additionally, access to antimalarials is inadequate in these remote locations.
In Nigeria, vaccines are typically rolled out through primary health centers, but of the 30,000 in the country, only about 20% are functional. Poor staffing, inadequate equipment, poor distribution of health workers, poor condition of infrastructure, and lack of essential drug supply continue to lead to ghost health centres. This means that the technical skill and infrastructure needed to administer the vaccine may be unavailable for many primary health centres.
There is also the issue of logistics. The cold-chain system of the country is made up of five strata; the National Strategic Cold Store (NSCS) which is the primary storage site for all vaccines in the country; six zonal stores located in each geopolitical zone in the country receive supplies from the NSCS; state stores receive supplies from zonal stores; Local Government Area (LGA) stores receive vaccines from their state store and the Primary Health Centres get supplies from the LGA store. The vaccine needs to be maintained at a temperature of 2-8 degrees celsius; the integrity of the cold chain must be unquestionable at every point of its journey until it is administered. Tertiary hospitals have been battling with incessant blackouts, and the national grid collapses almost every month. A vaccine that has not been maintained under the right conditions is as good as no vaccine at all.
The elephant in the room is vaccine hesitancy. Misinformation, religious and cultural beliefs and mistrust in conventional medicine prevents people from vaccinating their children. A cross-sectional study carried out in Southeastern Nigeria revealed that subjects who belong to a low socio-economic class were five times less likely to vaccinate self and baby with malaria vaccine when compared with those who were in a higher socio-economic class. Not even the tertiary-educated are exempted; up to 35.0% of undergraduates in a study conducted in Southwestern Nigeria responded that they would not take the COVID vaccine. No matter how many doses of the vaccine are made available, they can only get administered if they are accepted.
Charting the Path
The provision of the R21 vaccine is clearly a great step forward for Nigeria; the country with the largest cases of malaria in the world. But the road ahead is far from smooth. Studies would have to be carried out, policies made and innovative solutions explored to ensure that the vaccines produce the maximum effect.
The timing of the doses may not be adjustable, but all efforts must be made to ensure that children get all four doses. Wait times at immunisation clinics must be reduced to bare minimum. When Nigeria eradicated polio, it was because the oral polio vaccine was made so available and easy to administer. Community health workers took the vaccine to every home in the community, ensuring vaccine coverage for all. If malaria is to be eradicated (or at least reduced to a large extent in childlren), this approach must be employed again. The malaria vaccine is not as easy to administer, considering that it is an injectable, but mobile clinics can be organised at monthly intervals to deliver the vaccine to the doorstep of the children who need it most. Community pharmacists can also be involved in administering the vaccines at community level.
The vaccination distribution system needs to be redesigned. Rather than a central primary storage centre for all vaccines, vaccine collection should be decentralised, such that regional or state centres can receive vaccines directly from suppliers. Something similar has been tried during the COVID pandemic, through a 3-hub system involving Kano, Abuja and Lagos zonal storage sites receiving vaccines directly from suppliers and delivering them directly to states. Having a storage site in every region would reduce the bureaucracy associated with vaccine distribution. Strict surveillance and quality control, must of course be assured at all times.
The efficiency of the vaccine almost completely lies on the integrity of the cold chain. All health centres must have the capacity to store vaccines. Cold boxes must be made available, along with refrigerators that run constantly. Solar-powered fridges may be a good choice for remote locations that do not have access to electricity. Even in cities, refrigerators containing vaccines need a constant alternate supply to ensure the vaccines remain viable.
The malaria vaccine is not a magic jab. Other malaria prevention methods remain just as important, if not more important, in reducing the morbidity and mortality from this disease. Malaria control efforts must be taken on with more vigour. These include:
- Provision of insecticide-treated bed nets (ITNs),
- Encouraging indoor residual spraying (IRS) with insecticides,
- early diagnosis and treatment with antimalarial drugs, particularly artemisinin-based combination therapies (ACTs),
- intermittent preventive treatment in pregnancy to prevent complications from malaria in mothers and their unborn children,
- perennial malaria chemoprevention (PMC): giving malaria prophylaxis to children belonging to age groups at high risk of severe malaria), and
- seasonal malaria chemoprevention (SMC): giving prophylaxis to high-risk children at monthly intervals during the high malaria transmission season.
Finally, the eradication of malaria in Nigeria is possible. Other countries, including African countries have done it, even before the existence of the vaccines. Aggressive awareness strategies must be undertaken, to ensure that people even know that the vaccine is available. Targeted health education, infrastructure provision and structural adjustments would be required. Nigeria’s situation poses peculiar challenges, so solutions must be tailor-made. With a relentless approach, the malaria capital of the world can become malaria-free.
Aisha Ibrahim




