Specialist Clinic Ep. 1: Dental Health

So your teeth hurt when you take a cold drink. You hold your cheek with one hand and scrunch up your face. You let the pain fade on its own—it’s definitely not that serious. Or maybe it’s not even the cold drink. Your teeth just hurt every few days, and that’s when you remember to gargle your salt-and-water mixture. You occasionally remember to brush twice a day too.
This, unfortunately, reflects the attitude many Nigerians have toward their dental health.
Dental awareness in Nigeria is generally low. While many people understand the importance of brushing with toothpaste, knowledge of preventive measures like regular dental checkups, flossing, and the connection between oral health and overall well-being remains limited. Hence, our subject for today.
We introduce the first in our series: Specialist Clinic, where we’ll explore lesser-discussed aspects of personal health. We’ll raise awareness about them, especially within our campus community, visit relevant specialist clinics, and speak to professionals in the field. Today, we begin with dental health awareness.
A Look at the Numbers
Our first issue is the lack of data. Dental health in Nigeria is not only neglected by individuals, but also underrepresented as a subject matter. Only recently have public discussions on dental care begun to gain traction. Currently, there isn’t much statistical data available on oral health in Nigeria, but here are a few key insights:
- According to the 2012 National Oral Health Policy, between 6–23% of Nigerians have dental caries (tooth decay), and around 90% of these cases go untreated.
- Globally, about 100% of adults and 60–90% of schoolchildren experience tooth decay.
- As of 2022, Nigeria’s dentist-to-population ratio stood at 1:53,828, far from the WHO-recommended 1:5,000.
These numbers frame the problem we’re trying to explore. Dental health awareness in Nigeria remains significantly lower than in many developed countries. Challenges such as limited access to dental care, low utilization of available services, and poor public awareness continue to hinder progress. When we narrow our focus to the campus community, the pattern is no different: oral health awareness among students is equally poor. Let’s take a closer look.
Importance
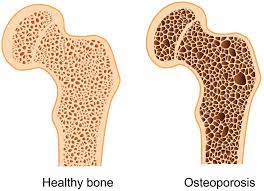
Dental health is crucial not only for maintaining oral hygiene but also for overall health and well-being. Within the mouth, good dental practices help prevent common issues like tooth decay (cavities), gum disease (gingivitis and periodontitis), and bad breath (halitosis). But beyond that, the mouth is often described as the “gateway to the body,” and for good reason.
Research shows that inflammation and infections caused by oral bacteria can contribute to serious conditions such as heart disease, clogged arteries, and stroke. Poor oral hygiene has also been linked to pneumonia, endocarditis, pregnancy complications like low birth weight and preterm labour, and even certain types of cancer. Oral infections can also worsen existing conditions like diabetes. Beyond the physical, oral health significantly impacts quality of life, affecting eating, speaking, and even social interaction.
So, how important are regular dental checkups? They’re key for both preventive and detective care. Routine dental visits help detect and prevent oral diseases, reduce the risk of tooth loss, and can even aid in the early detection of systemic illnesses. They also involve professional cleanings that reduce the buildup of plaque and prevent tooth decay and gum disease. The earlier an oral health issue is discovered, the easier and cheaper it is to treat. That’s why dentists recommend having a dental checkup every six months.
Status quo
Speaking with students across campus, it’s clear that most rely solely on brushing their teeth as their main form of dental care, usually once a day, and only twice when they remember. One in three students admitted they don’t know what flossing is; the rest only floss occasionally or when food is stuck. Mouthwash use is uncommon, and when asked why, students mentioned high cost or simply not seeing the need. Traditional methods like chewing sticks are no longer part of most students’ routines, although many said they used them as children. These habits fall far short of dental health guidelines, which recommend brushing twice daily with fluoride toothpaste and flossing at least once a day.
When it comes to dental pain or discomfort, students usually wait it out. Most do not visit a dentist unless the pain becomes unbearable. For instance, Faith*, who experienced sensitivity from a broken tooth, still didn’t seek professional care. This trend stands in contrast to the recommended standard of seeing a dentist every six months for preventive checkups and cleanings.
Interestingly, students with better awareness of dental health tend to be in related fields of medicine, dentistry, or allied health courses, though this awareness doesn’t always translate into better personal dental practices. Their academic exposure simply informs their understanding of oral health’s connection to systemic health. When asked about knowledge of dental checkup frequency, they were well aware of the six-month recommendation. In contrast, non-medical students like Faith, who tend to get information from social media, public campaigns, or word of mouth, see dental visits as only necessary when there’s a problem, mirroring how most people treat general health too.
A unique case was Kehinde*, whose sibling is a dentist. He receives regular checkups, understands his oral health better, and was diagnosed with congenital enamel hypoplasia, which makes him more prone to sensitivity. Because of this, he avoids cold drinks and follows up regularly. One can only wonder: how many others live with undiagnosed dental conditions?
But even for those who want to visit the dentist, there’s another barrier: they don’t know where to go. Faith couldn’t name a single dental clinic. Some students knew a few vaguely, but even medical students weren’t clear. Alarmingly, only 1 in 6 students knew that there’s a dental clinic in the university’s Jaja Clinic, and just a few could say exactly where it’s located.
Even when students know where to go, fear of the dentist is a barrier in itself. One in five admitted to fearing the machinery and procedures. Nnamdi, who had always been afraid, overcame his fear only after a recent visit. Simon* found his visit—out of curiosity—for scaling and polishing “unpleasant” and “uncomfortable” due to the instruments used. Still, not all experiences were negative, as Nnamdi, who went for an extraction, described his visit as “bittersweet”: “I went with the hopes that an extraction would be the last thing I’d do, but it turned out to be the perfect thing.” He also adds that the dental clinic he visited was really good with nice and hospitable doctors. For Kehinde, the visits feel more routine, though he admitted he would still rather not go if he had a choice. Left to their own decisions, many wouldn’t go at all.
Students who don’t seek dental care often cite: low priority, time constraints, and high costs. Laziness or disinterest and the bureaucratic stress of NHIS processes, especially for clinical students on the hospital campus. Among these, cost is perhaps the most pressing. Many students (and Nigerians at large) believe dental care is expensive: toothpaste and toothbrush prices, like every other thing, are rising, while floss and mouthwash are often seen as luxuries. As for procedures, Kehinde shared: “Scaling and polishing is fairly affordable, but everything else is expensive. I got a crown done for about ₦100,000 two or three years ago, but now it’s tripled.”
While NHIS (National Health Insurance Scheme) typically covers preventive care like cleanings and x-rays, it often doesn’t cover more intensive procedures like root canals or orthodontics. In a country with a minimum wage of ₦70,000, ₦150,000+ for a root canal or ₦1.2 million for a dental implant is out of reach for average citizens.
Cultural beliefs also shape attitudes toward dental care. In many communities, oral health literacy is low, and information access is poor. Traditional remedies still dominate. For instance, in parts of West Africa—and among some Muslim populations—chewing sticks are still used. Others believe checkups are unnecessary unless there’s visible damage or pain.
Some cultural misconceptions persist, such as the belief that cleaning your teeth loosens them or that tooth extraction can cause severe side effects. These beliefs create psychological barriers that keep people away from clinics, even when care is needed.
Voices from the Field: A Clinician’s Lens — The Jaja Dental Clinic
It may come as no surprise that the University of Ibadan’s health services include a dental clinic under the National Health Insurance Scheme (NHIS). But as highlighted earlier, most students are unaware that it even exists, let alone where it’s located. Given that dental care isn’t often seen as essential by students, it’s easy to understand how many pass through the university without ever discovering this facility. For those who don’t know, the Jaja Dental Clinic is located inside the Maternity and Intensive Care Unit building within the University Health Services (Jaja Clinic) complex and is open every day from 9 am. Just walk in and ask at the front desk for directions.

To better understand students’ dental health on campus, UIMSA Press spoke with Dr. Dada, a dentist at the Dental Clinic.
Q&A with Dr. Dada
Q: How would you describe the overall dental health awareness among students at the University of Ibadan?
Dr. Dada: The overall dental health awareness among students of the University of Ibadan was initially poor but is getting better as more students are now coming in for dental checkups and preventive measures, though a large number only visit the clinic when they have symptoms.
Q: What are the most common dental issues you see in students?
Dr. Dada: Most common are complications from untreated dental caries, such as dentoalveolar abscess, irreversible pulpitis, and acute apical periodontitis, which are conditions preventable with early intervention. Also commonly seen is Pericoronitis, a condition associated with impacted third molars, which is usually associated with the undergraduate age groups.
Q: What would you advise to change these?
Dr. Dada: Regular dental checkups every 6 months so that conditions can be prevented or measures taken to halt the progression of ongoing dental conditions.
Q: Do students generally seek preventive dental care or only visit when problems arise?
Dr. Dada: A large population of U.I. students come around when there are symptoms, usually pain. A very minute population comes in for preventive measures.
Q: What factors do you think influence students’ oral hygiene habits—stress, diet, cost, ignorance?
Dr. Dada: Oral hygiene habits depend on several factors, but mostly the patients’ dental awareness. Dental awareness modifies any personalised habits or conditions an individual may have, for example. When an individual knows that brushing twice daily, flossing, and visiting the dentist every 6 months improves his or her oral health and saves them from toothaches, frequent clinic visits and unwanted expenses, they will prioritise oral hygiene.
Q: Are there any particular oral health myths or misconceptions you often hear from students?
Dr. Dada: There is a belief that once you lose a tooth, it will be replaced by another. This is not true for adults who have lost their first set of teeth. Once the adult/permanent teeth are lost, they are never replaced.
Q: What role does the university play in promoting dental health awareness? Are there campaigns or outreach programs? What can be done?
Dr. Dada: The University management has done very well by establishing a dental clinic at the University Health Centre. This has helped create dental awareness for the students and made dental services accessible, from primary to tertiary care. More outreaches can, however, be organised in hostels, departments and even the students’ worship centres.
Q: It is found that a lot of students and even staff do not know of the presence of a dental clinic, and of the few that do, some do not even know where it is. What do you think about this? What do you think can be done to change it?
Dr. Dada: More oral health outreaches around campus would help spread awareness.
Q: What simple practices would you recommend for students to maintain good oral health, especially with tight schedules and limited funds?
Dr. Dada: Brush twice daily, floss regularly, and visit the clinic every six months.
Voices from the Field: A Researcher’s Perspective — National Dental Health
For a broader perspective beyond student life, we reached out to someone with dual experience—both as a dentist and a researcher. Dr. Omowunmi Femi-Akinlosotu shared her expert insights on the state of dental awareness, systemic challenges, and what can be done at both national and institutional levels.
Q: How often should people go for checkups, and how often do they?
Dr. Femi-Akinlosotu: This should be twice a year, every 6 months, though very few do this.
Q: What are the most common dental issues treated?
Dr. Femi-Akinlosotu: Generalised marginal gingivitis due to the accumulation of plaque and calculus on the teeth. When debris accumulates, it becomes calcified and hardens into calculus. Toothbrushing can’t remove these calculus, so the patient needs scaling and polishing. Another common dental issue is dental caries or cavities. This is especially among younger ones due to excessive consumption of carbonated drinks and sugary substances that demineralise the dental tissue. We also frequently see halitosis or bad breath.
Q: Do patients typically wait until they are in pain before seeking help?
Dr. Femi-Akinlosotu: Yes, they do. People do not go for regular dental checkups until they are experiencing severe pain which can no longer be relieved with analgesics, or when their issues begin to affect their aesthetics, relationships, or interactions with people. Sadly, this attitude cuts across all aspects of healthcare and not just dental health. Some even go to pharmacists for help. I believe this stems from a low level of awareness and poor literacy. We need health policies to curb this menace.
Q: What do you think about the awareness among Nigerians and UI students on dental care and health practices? Has it changed?
Dr Femi-Akinlosotu: Initially, dental health wasn’t taken seriously, but in the past 10 years, there has been an improvement in the awareness thanks to advocacy by the Nigerian Dental Association (NDA) across all states and the University of Ibadan Association of Dental Students (UADS) among UI students. Now, parents are concerned about the oral health and arrangement of teeth of their children, especially girls.
Q: Do you notice a difference in awareness or oral hygiene practices among age groups or regions?
Dr Femi-Akinlosotu: We’re not so good with data collection in this part of the world, so more research needs to be done to authenticate anything one has to say. As a researcher, I believe in data collection and research. With that, we can advocate for policy change and support from the government.
Q: What misconceptions about dental care do you frequently encounter?
Dr Femi-Akinlosotu: People think it’s very expensive, unaffordable and only meant for the rich.
Q: How affordable is dental care for the average Nigerian and student?
Dr Femi-Akinlosotu: Actually, dental care is not really affordable, especially for the lower cadre of the economy. I wish the government could subsidise more. It is why people patronise quacks and traditional remedies, which are not scientifically proven and might even cause more harm. For instance, for cases of oral lesions, these traditional remedies typically do not work and could make matters worse. Which is why I believe that while dental care isn’t cheap, nothing should be too expensive when taking care of one’s health.
Q: Are there policies present supporting or promoting oral health? Are they enough, if yes?
Dr Femi-Akinlosotu: As earlier mentioned, there has been more advocacy from the NDA, and policies have improved. There’s the NHIIS for workers and civil servants, and although initially, dental care was excluded because of the costs, some basic treatments have now been included. However, like Oliver Twist, I advocate for more.
Q: How do you think dental health ranks among Nigeria’s public health priorities?
Dr Femi-Akinlosotu: It’s not yet at the top, but we will get there. There are oral health implications tied to diseases of public health concern like HIV and mumps, which are spread easily, so there’s a need to better integrate oral health into the public health system.
Q: What would you suggest to improve the state of dental care in Nigeria and among students?
Dr Femi-Akinlosotu: First and foremost, we need to train more dentists in Nigeria to cater for our growing population. Only a few universities offer dentistry compared to the number offering Medicine and Surgery. It is very expensive to train a Dental Surgeon—the materials needed for one dentist could train about 10 physicians. Secondly, health professionals need more incentives and better remuneration. Many leave for better paying jobs and better working environments abroad. Thirdy, we need to boost awareness of among the people. Majority do not know that oral health issues detected by a dentist during routine examinations often reveal systemic ailments, allowing referral to the appropriate specialist.
For the University of Ibadan students, the Jaja Dental Clinic is already an added advantage. When I was a student, we didn’t have one. However, the clinic needs more staff to function optimally. The dentists there are seconded from UCH and are often overwhelmed. Also, many students and university staff do not even know that the clinic exists. I think Jaja needs to put out a memo and the dental students should engage in more campus advocacy during hall weeks and association events to make the UI community aware of the dental clinic.
Q: Do you think there are enough dental clinics available in the country?
Dr Femi-Akinlosotu: I do not have the data, but I’d say there isn’t. Establishing a dental clinic is expensive. A dental chair alone costs millions. Even though we have locally fabricated ones, it is not easy. We have a large population, so there’s still room for more. But even if we get this more, if people remain unaware of the importance of taking care of their oral health, we’d just open the dental clinics, and no one will visit.
Q: Do you think we are producing enough dentists in the country?
Dr Femi-Akinlosotu: We are not. In UI, the average number of students in a dentistry class is 25 to 30, which is small compared to the medical students’ 200. It is very expensive to establish a dental school, which is why most private universities do not offer it. We need more resources to establish more dental schools and produce more surgeons to cater to the populace.
Wisdom teeth
Next, we delved into a topic that is not too often discussed but affects everyone: wisdom teeth. Wisdom teeth, also known as third molars, are the last set of adult teeth to emerge, usually between the ages of 17 and 25. Positioned at the very back of the mouth (one on each side of the upper and lower jaws), they can erupt without issue for some people. However, for many others, there’s not enough space in the jaw to accommodate them, leading to a condition called impaction.
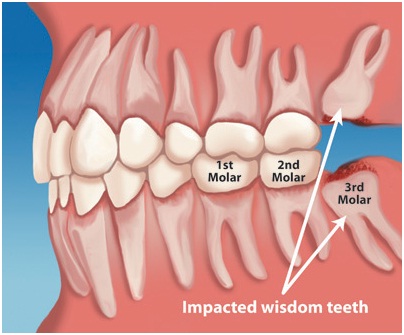
When wisdom teeth become impacted, they may grow at an angle, remain partially or fully trapped under the gums or jawbone, and lead to a number of problems, including pain, swelling, gum disease and infection, cavities, damage to neighbouring teeth, and in rare cases, cyst formation. Because of these risks, impacted or problematic wisdom teeth are often removed, especially if they’re causing pain or are likely to cause issues in the future.
Despite how common they are, wisdom teeth aren’t widely understood. From our campus conversations, 2 out of 5 students had no idea what a wisdom tooth is, and only a few barely remember when there’s erupted. Only 1 out of 5 had ever gotten theirs checked and had it removed.
We brought this up with Dr. Femi-Akinlosotu, who explained: “Some people have small jaws. When the permanent teeth, which are bigger than the milk teeth, start erupting. There might not be enough space to accommodate the new set of adult/permanent teeth. As a result, wisdom teeth often grow at an angle. Food gets trapped beneath, causing infection, inflammation, and eventually pain. Since wisdom teeth grow close to the pharynx, near the airway, infection in that area can be risky. It could spread or block the airway. That’s why we often advise patients to be very careful in taking care of their wisdom teeth.”
Q: Do you think people are informed enough about removing their wisdom teeth?
Dr Femi-Akinlosotu: There are a lot of myths. People say they don’t want to lose a tooth. So they ignore it until they have severe swelling or infections. This is why I stress the importance of advocacy. Dental pain can be excruciating. I’ve heard patients say it’s worse than labour pain. But they still don’t seek help until it’s unbearable.
Oral health in Nigeria
Outside the campus, dental clinics in Nigeria are unevenly distributed, with a higher concentration in the southern regions, particularly in Lagos. In contrast, the northern parts of the country have significantly fewer dental professionals and facilities, limiting access to oral healthcare for many. The government has made efforts to improve national dental care infrastructure through policies and programs, yet challenges persist.
The National Oral Health Policy, approved in 2012, was the first exclusive oral health policy in the country. It aims to improve oral health for 50% of Nigerians, emphasising early detection, immediate treatment, and awareness of oral diseases. Developed with multi-stakeholder input, the policy outlines strategies such as community-based awareness campaigns, early diagnosis and intervention, workforce development for oral health professionals, and better coordination of national oral health programs
Before the policy, the Community Oral Health Care Programme, launched in 1982 by the Community Dentistry Unit of the Faculty of Dentistry, University of Ibadan, had already begun addressing dental care needs in underserved communities. The program continues to play a dual role in both service delivery and training of dental professionals.
However, despite these frameworks, widespread oral health initiatives remain poorly implemented, especially at the grassroots level. According to Dr. Omowunmi Femi-Akinlosotu, the biggest barrier is funding:
“We need the government’s support so we can reach the rural areas and educate people about the importance of oral hygiene. Although we now have a speciality in dentistry called public oral health, we need more advocacy. In order to better integrate oral health into public health, we need the government to provide funding and also to legislate it. It’s not something you just barge into, so it needs to take effect from the federal level and then shift down to the state and local levels. When passed into law, it will become statutory.”
Moving forward
There’s no doubt that while awareness of dental care among students and Nigerians at large is gradually improving, it still falls short of what is necessary. There remains an urgent need for a deeper understanding of oral health, not just as a matter of aesthetics or discomfort, but as a critical part of overall well-being. Too many people stop at brushing twice daily or avoiding cold drinks, without fully grasping the importance of regular dental checkups or the connection between oral health and systemic diseases.
Moving forward, real progress must begin at the federal level. The government needs to better fund dental care infrastructure, support nationwide advocacy efforts, and integrate dental health more effectively into public health policy. At the same time, dental associations, both national and student-run, must continue to amplify awareness campaigns. Schools have a responsibility to include dental education in health curricula. Media and dental product advertisers can help shift the message from cosmetic benefits to health benefits, reinforcing that, in the words of Dr. Femi-Akinlosotu, “The mouth is the gateway to the body.”
Ultimately, every individual has a responsibility to take their oral health seriously, not only to avoid toothaches, but to safeguard their entire well-being.
*These are not the real names of the respondents, as they have chosen to remain anonymous.



This was a long but enlightening read 🔥🔥🔥. UIMSA press 🔥🔥🔥>>>