Emergency Series, Episode 4: Cardiac Arrest
It’s a regular afternoon. Lectures are ongoing, and everyone is tired. Then, suddenly, a student slumps over their desk and collapses. Their breathing stops, and they become unresponsive. Someone shouts for help: they do not think this was fainting. It could be a case of sudden cardiac arrest, a critical medical emergency which requires immediate action.
In this 4th episode of the Emergency Series, we will be exploring Cardiac Arrest: what it is, how to recognize it, what causes it, and most importantly, how to respond swiftly and effectively to save a life.
What is Cardiac Arrest?
Cardiac arrest occurs when the heart suddenly stops beating, or beats so fast that it fails to pump blood effectively. When this happens, the brain and other vital organs are starved of oxygen-rich blood, leading to loss of consciousness and, if untreated, death within minutes.
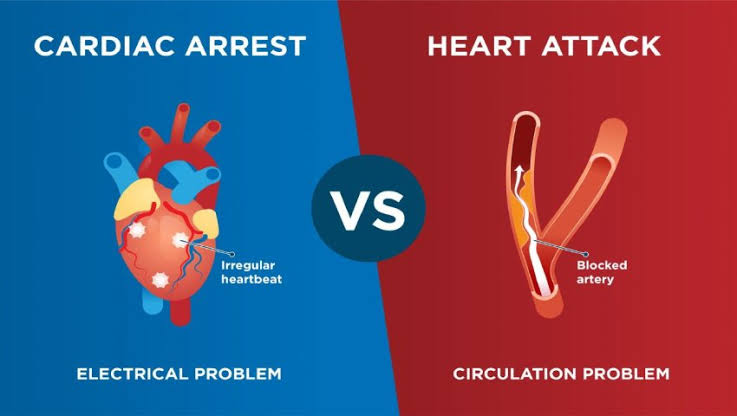
Although cardiac arrest is often confused with a heart attack, there’s a slight difference. A heart attack occurs when blood flow to a part of the heart is blocked while a cardiac arrest is caused by an electrical malfunction in the heart in which abnormal, rapid electrical impulses override the normal impulses. However, a heart attack can cause a change in the heart’s electrical activity that leads to sudden cardiac arrest.
When someone collapses suddenly, it can be difficult to distinguish between fainting and sudden cardiac arrest, but recognizing the difference is crucial. Fainting usually involves a brief loss of consciousness with a quick recovery, normal breathing, and a detectable pulse. In contrast, cardiac arrest causes immediate and prolonged unconsciousness, absence of breathing or abnormal gasping, and no detectable pulse. The skin may appear pale or bluish, and the person will not recover without immediate CPR and defibrillation. If there’s any doubt, it’s safest to assume cardiac arrest and begin emergency care right away, as every second counts.
Causes of Sudden Cardiac Arrest
Sudden cardiac arrest is most often caused by abnormal heart rhythms known as arrhythmias, particularly ventricular fibrillation (v-fib), where the heart’s electrical signals become chaotic and ineffective. These irregular rhythms can be triggered by various underlying conditions such as cardiomyopathies (diseases of the heart muscle), congenital heart defects, drug use, severe blood loss, respiratory failure, or certain infections. In some cases, medications for other health issues can also disrupt the heart’s rhythm. These disturbances prevent the heart from pumping blood effectively, leading to a sudden and life-threatening collapse.
Emergency Response: What to Do?
- Call for emergency medical help while you assess the individual.
- Start Cardiopulmonary Resuscitation (CPR) immediately using hands only or an Automated External Defibrillator (AED):
- Place both hands on the center of the chest (at the sternum, just above the apex beat).
- Perform about 30 chest compressions at a depth of at least 4–5 cm.
- Assisted breathing can also be done after every 30 compressions.
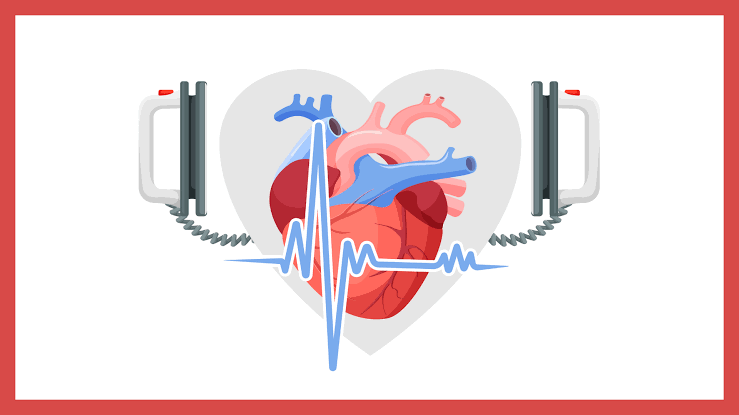
- Once emergency personnel arrive, defibrillation can restart the person’s heart if they haven’t received a shock from an AED yet. Defibrillators shock the heart through paddles placed on your chest. The current travels to the heart. This stops the abnormal impulses and restores the normal impulses that make it beat. It may take more than one shock for the heart to pump on its own again.
CPR plus Defibrillation can rescue someone from sudden cardiac arrest especially. The shorter the time between arrest and defibrillation, the higher the chance of survival.
Advanced medical care
The emergency personnel might then give the person intravenous antiarrhythmic drugs to regulate heart rhythm before transferring them to a hospital to take care of complications that may have occurred from the incident.
These complications can range from broken ribs, to fatigue, or even brain damage; hypoxic brain damage is the most common and life threatening due to lack of oxygen.
Diagnosis and Monitoring
Sudden Cardiac arrest is diagnosed with the symptoms present as there’s little time for tests and evaluation. These symptoms includes fatigue, light headedness, chest pain, nausea, shortness of breath, loss of consciousness etc. The most common of these is chest pain, however, it is often ignored as it can be a symptom of other diseases.
The survival rate drops by approximately 10% with every minute of delay in initiating treatment. However, survival can be as high as 90% when CPR and defibrillation are initiated within the first minute.
Conclusion
Sudden cardiac arrest is one of the most time-sensitive emergencies in medicine. Immediate recognition, CPR, and defibrillation are the cornerstones of survival. Understanding the signs, knowing how to respond, and being prepared to act could be the difference between life and death for someone in need.